Navigating the Complex Interplay of Obesity and Diabetes: Strategies for Prevention, Management, and Overall Well-Being
INTRODUCTION
In the modern world, two pervasive health issues, obesity and diabetes, have emerged as major public health concerns. These conditions are closely intertwined and often coexist, creating a complex and multifaceted challenge for individuals and healthcare systems alike. In this comprehensive article, we will explore the definitions of obesity and diabetes, dissect the intricate relationship between the two, and delve into effective prevention and management strategies, all while emphasizing the importance of overall well-being.
Part 1: Understanding Obesity
1.1 What is obesity?
Obesity is a chronic medical condition characterized by an excess accumulation of body fat. It is typically assessed using the Body Mass Index (BMI), which considers an individual’s weight in relation to their height. Obesity is medically defined as having a Body Mass Index (BMI) of 30 or greater.

1.2 The Causes of Obesity:
Obesity can stem from various factors, including genetic predisposition, environmental influences, and lifestyle choices. Key contributors to obesity include:
a) Poor Diet: Consuming high-calorie, low-nutrient foods can lead to weight gain.
b) Lack of Physical Activity: Sedentary lifestyles with minimal exercise can contribute to obesity.
c) Genetics: Genetic factors can influence an individual’s susceptibility to obesity.
d) Psychological Factors: Emotional eating and stress may contribute to overconsumption and subsequent weight gain.

1.3 Health Consequences of Obesity:
Obesity is linked to a spectrum of health issues, which encompass:
a) Type 2 Diabetes: Obesity is a major risk factor for the development of type 2 diabetes.
b) Cardiovascular Disease: Obesity increases the risk of heart disease, hypertension, and stroke.
c) Joint Problems: Excess weight places strain on joints, leading to conditions like osteoarthritis.
d) Mental Health Issues: Obesity can contribute to depression and low self-esteem.
Part 2: An Insight into Diabetes
2.1 What is diabetes?
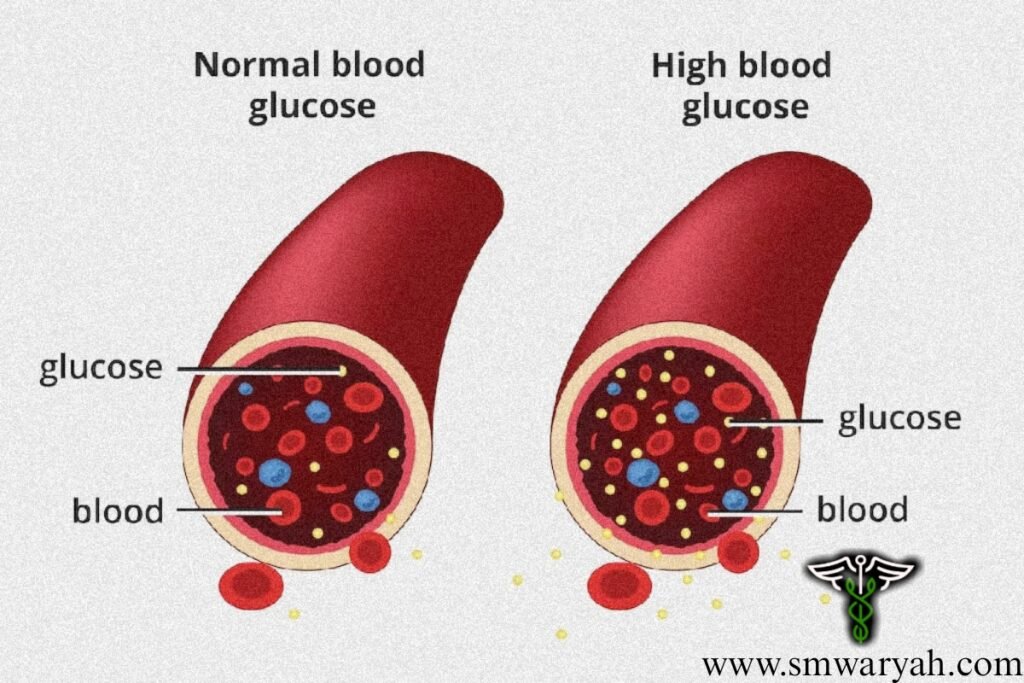
Diabetes is a group of metabolic disorders characterized by elevated blood sugar levels over an extended period. Diabetes primarily manifests in two distinct forms:
a) Type 1 diabetes: an autoimmune condition where the immune system attacks and destroys insulin-producing cells in the pancreas. This results in a lack of insulin, necessitating lifelong insulin therapy.
b) Type 2 Diabetes: Linked to lifestyle factors, type 2 diabetes occurs when the body becomes resistant to insulin or fails to produce sufficient insulin to maintain normal blood sugar levels. It is often associated with obesity and can sometimes be managed with lifestyle changes and medications.
2.2 CAUSES OF DIABETES:
The causes of diabetes vary between the two main types:
a) Type 1 diabetes: thought to be triggered by genetic and environmental factors, although the exact cause is still unknown.
b) Type 2 Diabetes: Lifestyle factors, such as poor diet, lack of exercise, and obesity, play a significant role in the development of type 2 diabetes.
2.3 HEALTH CONSEQUENCES OF DIABETES:
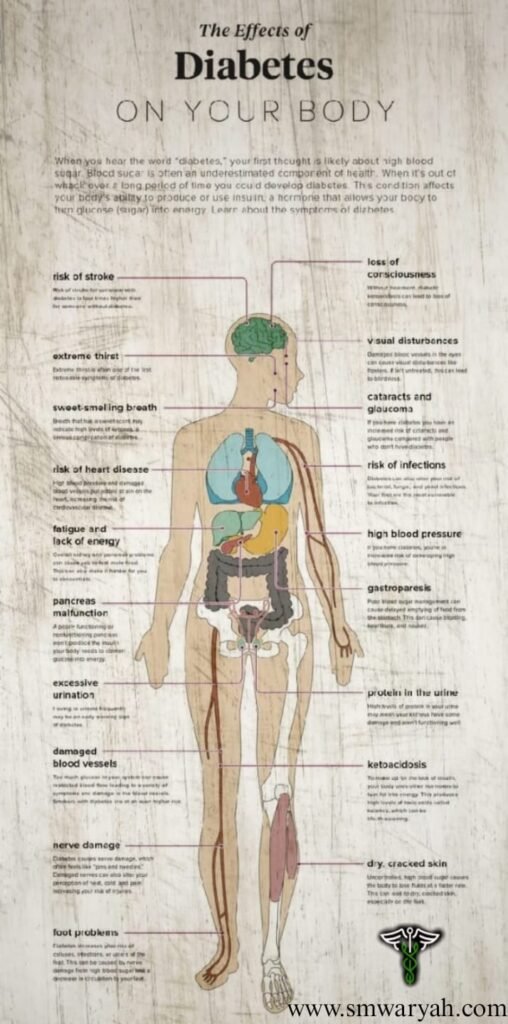
Uncontrolled diabetes has the potential to result in significant complications, including:
a) Cardiovascular Issues: Diabetes increases the risk of heart disease, stroke, and hypertension.
b) Kidney Disease: High blood sugar levels can damage the kidneys, leading to kidney failure.
c) Vision Problems: Diabetes can cause retinopathy and potentially lead to blindness.
d) Nerve Damage: Peripheral neuropathy can result in pain and numbness in the extremities.
Part 3: The Complex Relationship Between Obesity and Diabetes
3.1 Obesity as a Precursor to Type 2 Diabetes:
Obesity stands out as a significant and prominent risk factor for the development of type 2 diabetes. Excess body fat, particularly abdominal fat, can lead to insulin resistance, a condition where the body’s cells do not respond effectively to insulin. This forces the pancreas to produce more insulin to compensate, ultimately resulting in high blood sugar levels and the development of type 2 diabetes.
3.2 Diabetes Exacerbating Obesity:
The relationship between diabetes and obesity is complex and bidirectional. Diabetes management often involves insulin or medications that can lead to weight gain. Additionally, fluctuating blood sugar levels can result in fatigue and reduced physical activity, making it challenging to maintain a healthy weight.
3.3 Shared Risk Factors:
Obesity and diabetes share several risk factors, such as genetics, a sedentary lifestyle, poor dietary choices, and stress. These common factors further complicate the relationship between the two conditions.
Part 4: PREVENTION OF OBESITY & DIABETES
4.1 Lifestyle Modifications:
Preventing obesity and diabetes often begins with lifestyle modifications.
a) Healthy Eating: Adopting a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help control weight and blood sugar levels.
b) Regular Physical Activity: Incorporating regular exercise into your routine can improve insulin sensitivity and aid in weight management.
c) Stress Management: High stress levels can contribute to overeating and poor food choices. Practicing stress-reduction techniques like meditation or yoga can be beneficial.
4.2 Weight Management:
Maintaining a healthy weight is crucial to preventing both obesity and type 2 diabetes. Setting realistic weight loss goals and seeking guidance from a healthcare professional or registered dietitian can be highly effective.
4.3 Diabetes Prevention Programs:
For individuals at high risk of developing type 2 diabetes, participating in diabetes prevention programs can be invaluable. These programs often combine lifestyle changes with education and support.
4.4 Medication and Insulin Therapy:
In some cases, medications or insulin therapy may be necessary to manage diabetes. Collaborating closely with a healthcare provider is crucial in devising an individualized and effective treatment strategy.
Part 5: Managing Obesity and Diabetes While Emphasizing Overall Well-Being
5.1 Medical Supervision:
If you are already dealing with obesity and diabetes, it’s crucial to work closely with healthcare professionals to manage both conditions effectively. Regular check-ups, blood sugar monitoring, and medication adjustments may be necessary.
5.2 Individualized Approach:
Each person’s experience with obesity and diabetes is unique. Tailoring treatment plans to an individual’s specific needs and goals is essential for long-term success.
5.3 Support and Education:
Support groups and educational resources can provide valuable information and emotional support for individuals managing obesity and diabetes. Empowerment often arises from connecting with individuals who share similar challenges and experiences. 5.4 Embracing Overall Well-Being:
While tackling obesity and diabetes is crucial, it’s equally important to focus on overall well-being. Prioritizing mental health, seeking balance in life, and nurturing positive relationships can enhance the journey toward better health.
CONCLUSION
Obesity and diabetes represent significant health challenges in today’s world, and their complex relationship necessitates a multifaceted approach to prevention and management. Understanding how these conditions interplay and adopting a healthy lifestyle can help reduce the risk and enhance the quality of life for individuals affected by obesity and diabetes. By embracing overall well-being, including physical, mental, and emotional health, individuals can navigate this complex interplay more effectively and work towards a healthier and more fulfilling life. Remember, with the right knowledge, support, and commitment, both prevention and management are achievable, paving the way toward a brighter future.